There truly is a huge cost associated with entitlement programs. Nothing is "free" in this world. If you're not paying for something, someone else is paying for it in some way or another. That's all great until the people who are paying for everything run out of money themselves. Unfortunately, I'm afraid that time is coming, sooner than you think.
Here's one example where entitlement is wrong:
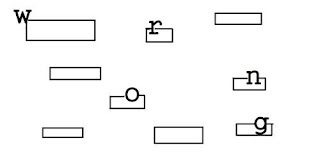
This is a portion of a label that prints when we process a prescription. It also has the patient and prescriber information (not shown) as per state board of pharmacy requirements. This is affixed to the back of the prescription.
As seen above, it has the name of the drug, quantity, NDC (National Drug Code), instructions, and some pricing information. That's what I'd like you to notice...
With THIS prescription, OUR cost is $40.88. That's just for the medication. The price of the label, bottle, cap, cost to adjudicate, shipping fee, cost for tech, pharmacist, etc... would all be on top of that. Granted, it's not very much per prescription, but it does add up over time.
So what's the point? The point is that THIS prescription was processed on MEDICAID, a state-funded program for low income people. My pharmacy was reimbursed from Medicaid $31.40. That means with this prescription we lost $9.48 BEFORE all the other overhead and variable costs I mentioned. Further, due to the way Medicaid is set up, the pharmacy has no choice in the matter... no way to fight it. There's nothing the pharmacy can do about it. This type of reimbursement doesn't happen with every prescription on Medicaid, but it happens enough (in my mind) to matter. With many other prescriptions on Medicaid, the reimbursement is so little over cost that when you add in the variable costs it turns out to be a wash in most cases.
Just so you know... ANY business MUST make a profit to STAY in business. If you truly don't understand that concept, you need to open a lemonade stand this weekend and figure it out on your own. The MORE people that go on state-funded Medicaid programs, the MORE this happens. The MORE this happens, the LESS profit there will be for the pharmacies involved. In that case, businesses will seek other ways to make up the deficit, and that will be higher prices for every day items. This means that people who are paying the taxes to pay for people on Medicaid will incur extra costs hidden in everyday items at the grocery or pharmacy.
There's another factor associated with this entitlement... when a company is forced to work with less profit, the first thing they cut is the work force. As a result of less profit, my Goofmart pharmacy reduces tech hours. A reduction in tech hours puts more of the workload strain on pharmacists. That in turn leads to a higher rate of error. Eventually that will end up with a patient being seriously harmed. This is not conjecture. This is reality.
No one wants truly poor people to be hungry or not get their medication. There are people who truly need our help until they get back on their feet and can contribute to society and making a living for themselves. Unfortunately, the system doesn't police who is truly indigent and those who are taking advantage of the system (see EXAMPLE).



7 comments:
1) Are you more upset that the pharmacy is losing money or that the script is for Oxy?
2) Can a pharmacy refuse to fill scripts for drugs it loses money on?
3) Can a pharmacy insist that the client pay the difference? Under any circumstances or under only some? If they can do this, why don't they?
4) Can a large pharmacy chain negotiate prices with suppliers to avoid having this happen?
5) Is having a pharmacy remunerative enough (for other drugs or because it draws customers) that a loss on some drugs is the cost of doing business?
6) Can a pharmacy refuse to fill scripts for people with medicare/medicaid (or whatever gov't plan applies), the way some doctors refuse medicare patients...or refuse to bill insurers.
I have only been in business for year and a half and I have seen reimbursements on some plans including Medicaid be reduced substantially. I have negative profits on 8%of my rxs on a daily basis. mind you that it may be only a couple of bucks but that adds up real quick. Medicaid pays horrible but MEdimpact and Medco have some plans that a ridiculous. I have spent a couple thousand dollars on a 90 day brand drug and lost $2.50. A bit disheartening to say the least. Pharmacies are making smaller margins than any business that I am aware of. Yet Medco, CAtamaran, Medimpact are making BILLIONS as middle men that don't seem to add much to the delivery of healthcare. With take or leave it contracts and almost no oversight on these companies, I fear we have not seen the bottom yet
1) Are you more upset that the pharmacy is losing money or that the script is for Oxy? The drug itself is irrelevant. Pharmacies receive negative reimbursements on all types of drugs, even antibiotics.
2) Can a pharmacy refuse to fill scripts for drugs it loses money on? It depends on the chain. My store allows a negative reimbursement of up to $50.00 per script. I have to do everything I can to reduce the negative, such as filling fewer tablets, or looking at different manufacturers.
3) Can a pharmacy insist that the client pay the difference? Under any circumstances or under only some? If they can do this, why don't they? We can in theory, but the customer rarely is agreeable to this arrangement.
4) Can a large pharmacy chain negotiate prices with suppliers to avoid having this happen? This question is very, very complex. Chains and suppliers DO negotiate prices. This is why the pharmacy is always changing manufacturers. Whatever brand is the lowest negotiated price is the pharmacies "preferred" brand. It is when he insurance gets involved that things become tricky, because the insurance operates on something called AWP- the average wholesale price. This means that we are not reimbursed based on the actual price paid, but rather on the AWP. So, if the pharmacy paid LESS than the AWP price, we make money. In the absolute most basic terms, But if we paid MORE than AWP, we lose money. It is far more complicated than that in actuality.
5) Is having a pharmacy remunerative enough (for other drugs or because it draws customers) that a loss on some drugs is the cost of doing business? It depends. CVS, for example, does so much business that they don't worry overmuch about individual losses, because volume takes care of it. That's why the are so aggressive about refills. Smaller chains and independents are affected dramatically. Most of the time, the profit margin is literally only a few cents. SOMETIMES, the profit is hundreds of dollars. We are pretty happy to see profits of 5 bucks per prescription, and that's the truth.
6) Can a pharmacy refuse to fill scripts for people with medicare/medicaid (or whatever gov't plan applies), the way some doctors refuse medicare patients...or refuse to bill insurers. Yes and No. As long as the chain has a contract with the insurance company, we have to do our best to fill them even with the loss. However, there have been occassions when pharmacies refused contracts with certain insurance companies because of reimbusement rates, such as Express Scripts and Walgreens.
Ah, so it *not* just the PCRS (Ireland) who think this works as an idea.
Main social insurance scheme here repays at 92% of cost + a fixed dispensing fee, so on particularly dear products and basically all fridge products, you lose money. The part-funded scheme has just gone from 120% to 100% and I'm expecting it to go to 92% pretty damn soon too...
When IN first went to a $3 Copay on mediciad, we were told if patient said they couldnt pay we couldnt make them, just collect copay slips and try and bill at end of month....course u see where that went. Then we started telling them they had to pay even if not right rules. all of chains made them pay so why couldnt we as independent. Sorry if you can have a nicer smartphone than me, drive a newer car than me and get you hair and nails done to the nines
....you can fork out 3 bucks for your xanax and vicodin which is a whole nother topic
yes a pharmacy can refuse to bill medicaid plans if they are private hmos that did not come to an agreement with pharmacy. case in point: Molina is a company that runs medicaid hmos in several states, they just got into south carolina and walgreens refused to contract with them. so no molina customers for the WAG in sc.
Your insurance company pays you back your full reimbursement as long as it's within 7 days of receipt .I had the same problem with Darby pharmacy called my insurance they sent me a check for what I paid outta pocket ....Hope this helps
Post a Comment